Abstract
Introduction: Preclinical data suggest that PD-1 and PD-L1/PD-L2 mediate immune evasion in CLL. However, clinical data (Ding, BLOOD 2017) demonstrate that pembrolizumab monotherapy (pembro) is ineffective in relapsed/refractory (r/r) CLL patients (pts) (ORR 0%, med PFS 2.4 months). Additional data with an anti-PD1 demonstrated a 90% failure rate in Richter's Transformation (RT) with a med 2-month OS (Rogers, BJH 2018). Combinations may represent the future of anti-PD-1 therapy in CLL/RT, especially in RT pts rel/ref to ibrutinib, where median OS is ~3.5 mos. We hypothesized synergistic activity with PD-1 + PI3K blockade. Umbralisib (UMB), is a highly-specific PI3K-δ inhibitor with additional effects on casein kinase-1 epsilon (CK-1ε), which may have an inhibitory effect on Treg function (Deng et al, 2016). We tested the safety and activity of UMB in combination with the anti-CD20 mAb ublituximab (UTX) and pembro in r/r CLL and RT - the first reported combination of a PD-1 inhibitor + PI3K-δ inhibitor in this population.
Methods: Ph I (3+3 design), multicenter study to assess the safety/efficacy of UMB + UTX + pembro in pts with r/r CLL and RT. Treatment for CLL pts involved three stages: Induction: UMB (800mg daily) and UTX (900mg 3 out of 4 wks) for the first two 28-day cycles. Consolidation: Pembro (dose level 1=100mg, dose level 2=200mg) was then initiated every 3 wks in combination with UMB and UTX (900mg week 2 of cycle 4 and 6) for cycles 3-6. Maintenance: Cycle > 6, UMB 800 mg daily until progressive disease (PD) or unacceptable AE. For RT pts, all study drugs are started in cycle 1 with the following schedule: UMB 800 mg daily; UTX 900 mg cycle 1 (D1, 8, 15), D1 cycles 2-4, cycle 7 and q3 cycles thereafter; and pembro D3 of cycle 1 and D2 of cycles 2-4. The primary endpoint is safety of the triple combination with efficacy as a secondary endpoint. Response assessments for CLL, based on the iwCLL 2008 criteria, were performed after cycles 2, 6 and 12. RT response assessments (Cheson 2007) were completed at the end of cycles 2, 4 and every 3 cycles until month 12. Peripheral blood and/or bone marrow biopsy, enriched for mononuclear cells, were obtained for correlative analyses at screening, month 2 and 6.
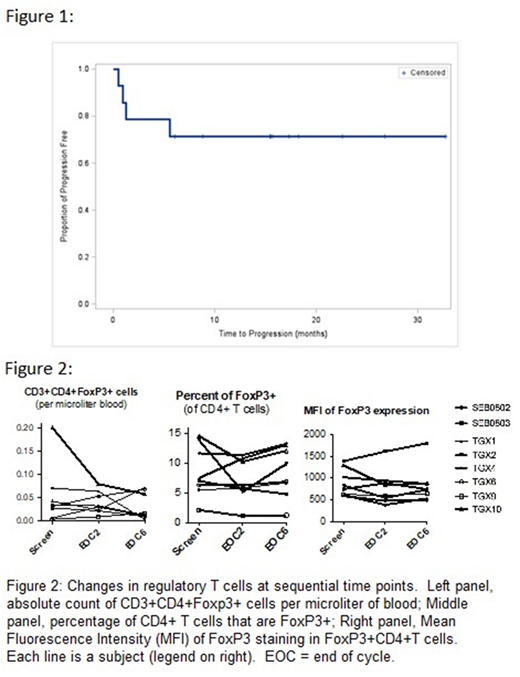
Results: Fourteen pts have been treated to date: 9 with CLL (3 at 100 mg pembro / 6 at 200 mg pembro) and 5 with RT (4 at 100 mg pembro / 1 at 200 mg). Baseline demographics were as follows: male/female (9/5), med age 71 yrs (range 60-81), med prior therapies 2 (1-8), 79% were refractory to immediate prior therapy. 10 pts had prior ibrutinib of which 9 were ibrutinib refractory. 64% of pts had at least 1 high risk genetic feature (del17p, del11q, TP53 mut, NOTCH1 mut or complex karyotype). AE's (all causality) were manageable. Grade 3/4 AE's occurring in ≥ 3 pts included neutropenia (n=6, 43%), ALT/AST increase (n=3, 21%) and hypophosphatemia (n=3, 21%). One DLT occurred in a CLL pt at 200 mg dose level (ALT/AST elevation) which trigged expansion to 6 pts. No additional DLTs were reported, and no MTD was achieved. No increase in expected grade ≥ 3 PI3Kδ-associated toxicities were noted (1 pneumonitis event, no colitis events). ORR was 89% for CLL pts with ORR of 75% in BTK refractory CLL pts (3/4). Notably 2/4 BTK refractory CLL pts achieved a response to UMB + UTX (U2) induction alone prior to the addition of pembro. 4/5 RT pts were eligible for efficacy evaluation with 50% ORR (2/4, CR). The 2 RT CRs were durable and are ongoing (15+ mos and 7+ mos); both pts were ibrutinib refractory and had 7 (including SCT) and 8 prior lines respectively, and one had failed CAR-T. With a med follow up of 15 mos, 10/14 (71%) remain progression free (range 3 - 44 mos, Fig 1), including one CLL pt who completed consolidation and has been off therapy for 27+ mos. Sequential sampling for correlative studies demonstrated modest changes in Tregs numbers (Fig 2).
Conclusion: The triplet combination of umbralisib + ublituximab + pembro was well-tolerated. Responses were durable in BTK refractory, high risk pts, including two CR's in RT pts. In contrast to pembro monotherapy, data suggest that CLL/RT pts who achieve ≥ PR with this checkpoint inhibitor-containing regimen can achieve durable responses. Correlative studies suggest that maintenance of Tregs may limit autoimmune sequelae. Enrollment is ongoing in both the CLL (BTK refractory only) and RT cohorts.
Mato:AbbVie: Consultancy, Research Funding; Portola: Research Funding; Regeneron: Research Funding; AstraZeneca: Consultancy; Johnson & Johnson: Consultancy; Celgene: Consultancy; Medscape: Honoraria; TG Therapeutics: Consultancy, Research Funding; Pharmacyclics, an AbbVie Company: Consultancy, Research Funding; Acerta: Research Funding; Prime Oncology: Honoraria. Svoboda:Regeneron: Research Funding; KITE: Consultancy; Bristol-Myers Squibb: Consultancy, Research Funding; TG Therapeutics: Research Funding; Pharmacyclics: Consultancy, Research Funding; Kyowa: Consultancy; Seattle Genetics: Consultancy, Research Funding; Merck: Research Funding. Schuster:Gilead: Membership on an entity's Board of Directors or advisory committees; Novartis Pharmaceuticals Corporation: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Nordic Nanovector: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy, Honoraria, Research Funding; Dava Oncology: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Genentech: Honoraria, Research Funding. Becker:GlycoMimetics: Research Funding. Brander:DTRM: Other: Institutional research funding for non investigator initiated clinical trial, Research Funding; BeiGene: Other: Institutional research funding for non investigator initiated clinical trial, Research Funding; Novartis: Consultancy, Other: DSMB; Pharmacyclics, an AbbVie Company: Consultancy, Honoraria, Research Funding; Acerta: Other: Institutional research funding for non investigator initiated clinical trial, Research Funding; TG Therapeutics: Consultancy, Honoraria, Other: Institutional research funding for non investigator initiated clinical trial, Research Funding; Teva: Consultancy, Honoraria; Genentech: Consultancy, Honoraria, Other: Institutional research funding for non investigator initiated clinical trial, Research Funding; AbbVie: Consultancy, Honoraria, Other: Institutional research funding for non investigator initiated clinical trial, Research Funding. Dwivedy Nasta:Aileron: Research Funding; Pharmacyclics: Research Funding; Debiopharm: Research Funding; Incyte: Research Funding; Rafael/WF: Research Funding; Roche: Research Funding; Takeda/Millenium: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Merck: Other: DSMC. Landsburg:Takeda: Consultancy; Curis: Consultancy, Research Funding. Kennard:AbbVie, Gilead, Verastem: Consultancy. Zelenetz:Abbvie: Research Funding; Celgene: Consultancy; AstraZeneca: Consultancy; Novartis/Sandoz: Consultancy; Amgen: Consultancy; Gilead: Consultancy, Research Funding; Genentech/Roche: Consultancy, Research Funding. Purdom:TG Therapeutics: Employment, Equity Ownership. Paskalis:TG Therapeutics: Employment, Equity Ownership. Sportelli:TG Therapeutics: Employment, Equity Ownership. Miskin:TG Therapeutics: Employment, Equity Ownership. Weiss:TG Therapeutics: Employment, Equity Ownership. Shadman:Gilead Sciences: Research Funding; Celgene: Research Funding; AstraZeneca: Consultancy; Beigene: Research Funding; AbbVie: Consultancy; Genentech: Research Funding; Qilu Puget Sound Biotherapeutics: Consultancy; Genentech: Consultancy; Mustang Biopharma: Research Funding; Acerta Pharma: Research Funding; TG Therapeutics: Research Funding; Pharmacyclics: Research Funding; Verastem: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal